Understanding Mentoring in Surgery, Takeovers and Telestration
People involved
Solène Lambert

Abstract
This project focuses on surgical mentoring. All along their careers, surgeons learn through mentoring, operating on patients side-by-side with expert surgeons. However, access to experts is more and more challenging as they are often located far from learners. Telementoring can increase the reach of mentors by supporting mentoring at a distance, but despite their potential, current systems remain rarely institutionalized. Moreover, the physical distance between mentors and mentees poses unique challenges to remote surgical training.
In a first paper, we investigate current surgical mentoring practices, to inform future design of telementoring systems in providing support for learning. In a field study, we observe 11 surgeries and conduct follow-up self-confrontation interviews with mentor-mentee pairs. Through Thematic Analysis, we find that the domain of surgery results in mentee's needs for reassurance regarding safety, being spared from workload and risk, both essential to support the acquisition of skills. Second, that mentors understand the situation primarily through the surgical site view but also through inspecting the mentee's posture and the patient's body. Thirdly, that mentors take physical distance as their presence limits mentees' autonomy development. We discuss the limits of current surgical telementoring systems and rethink their role as companions of onsite mentoring.
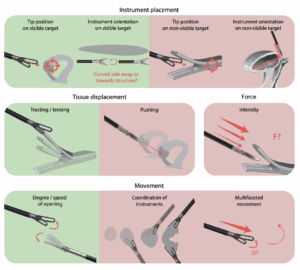
In a second paper, we investigate the underlying needs leading to takeovers in onsite mentoring and assess mentors’ ability to fulfil address these needs remotely using existing telestration tools, namely pointers and drawings on shared views. Through interviews and workshops with expert surgeons, we find that (1) mentors take over to convey gestures related to instrument placement, tissue displacement, force, and movement, (2) mentors gather information about location of tissue, equipment, and instruments, as well as gesture constraints, and (3) surgeons judge telestration insufficient for these needs. Based on this gap between onsite mentoring practices and telementoring tools, we discuss novel tools to address these needs and their evaluation.
Project description
Papers:
https://dl.acm.org/doi/abs/10.1145/3637420
https://dl.acm.org/doi/abs/10.1145/3613904.3641978